Table of Contents
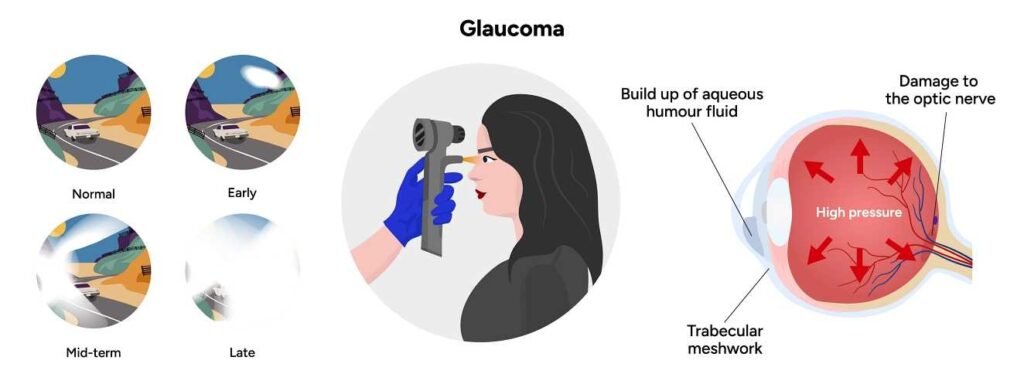
People do not often discuss glaucoma, but it affects millions of individuals around the world. Recent estimates show that over 80 million people around the globe had glaucoma in 2020. Analysts expect this number to increase to more than 111 million by 2040.
We must address this issue for the betterment of millions of people and the planet. No one wants to struggle with something a doctor could have diagnosed sooner.
The latest developments in the field promise significant improvements in testing and diagnosis. Medical professionals can now more quickly and easily identify glaucoma in patients, helping them recommend practical solutions to ease symptoms.
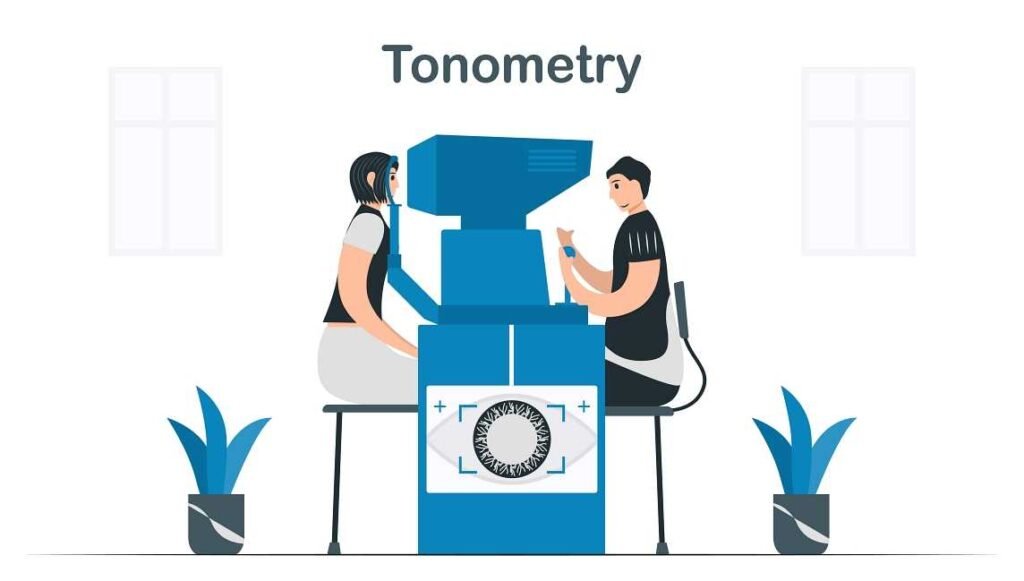
A critical piece of equipment for professionals is the tonometry devices. Today, we will focus on these devices. We will look at how glaucoma care practices are changing.
What is a Tonometry Devices?
When a patient visits an optometrist’s office, they must undergo several tests to check their eye health. One such test involves the use of a tonometry devices. The Cleveland Clinic explains that a tonometry test is a simple and fast way to check for glaucoma.
Tonometry refers to a type of eye test that measures pressure inside your eye (intraocular pressure). A doctor performs one of the essential glaucoma tests. A few different methods and ways to do this test exist, all quick and painless.
These devices measure the pressure inside a patient’s eye. The designers also create them to be comfortable for the patient. This is to say that all patients who undergo this kind of examination should feel comfortable while they are taking the test.
After all, there is nothing worse than feeling out of sorts while at a doctor’s office. The tonometry devices provides quick and accurate readings of intraocular pressure. This helps the optometrist make follow-up recommendations immediately.
Which Types of Tonometry Testing are Available?

Not everyone uses the same tonometry testing method. Rather, a multitude of testing options exist for optometrists to select from depending on their patient’s specific needs. Among those testing methods include the following:
- Continuous Monitoring – This option is available for certain patients who may require constantly updated readings of their eye pressure. A more advanced tool for measuring eye pressure exists. You wear a sensor on your eye, like a contact lens. This sensor feeds data back to the optometrist’s office for constant monitoring of the patient’s eye pressure.
- Applanation Tonometry – If other eye pressure tests show unusual results, an optometrist may use applanation tonometry. This test helps find the true eye pressure. This is because applanation tonometry is concerned to be among the most accurate tests of one’s inner eye pressure.
The device in this test determines how much pressure you must apply before your eye surface begins to flatten. This method helps you determine whether you need a lot of pressure to cause this reaction. If that is the case, this may be a sign of issues with glaucoma.
- Non-Contact Tonometry – A popular option in many optometrists’ offices these days is a non-contact tonometry test. This is because many patients are not thrilled with the concept of something directly touching their eyeball just to get a test result. Instead, they prefer a machine that doesn’t have to make any direct contact with their eyes at all.
The non-contact tonometry test uses a small puff of air blown into the eyes. This quick test checks how the eyes respond. A healthy eye reacts quickly to an invasion. However, if it does not react, a person may have glaucoma or another problem.
These are just some of the test types that an optometrist might order for his or her patient. They will decide based on the resources they have and the preferences of each patient. Combining those two factors is always best. This helps choose the best testing type for each person who comes to the office.
Who is Most at Risk for Glaucoma?
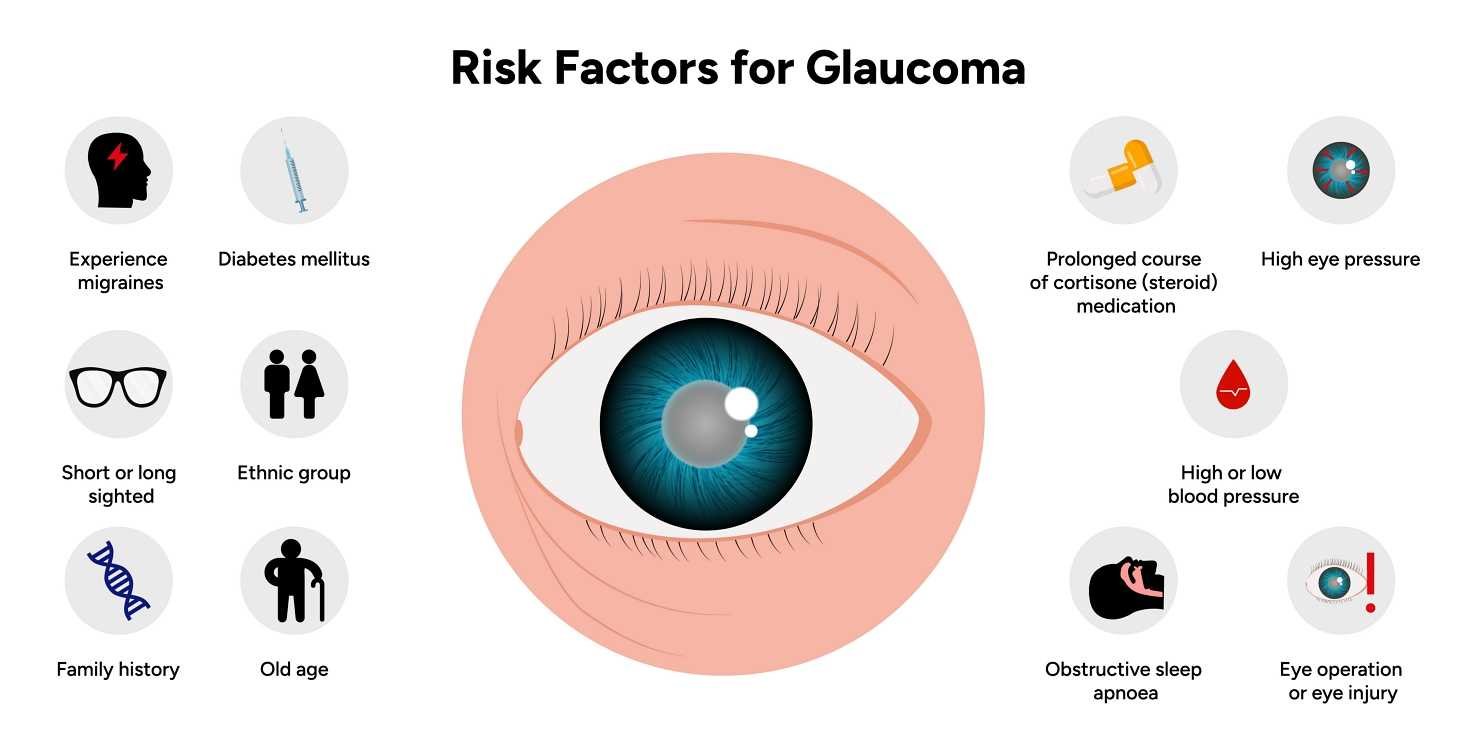
 Anyone can develop glaucoma, but some groups should pay more attention to this risk. Those who fall into exceptionally specific categories are more likely to experience this issue. The American Academy of Ophthalmology (AAO) states that the following groups are at particularly high risk of glaucoma:
Anyone can develop glaucoma, but some groups should pay more attention to this risk. Those who fall into exceptionally specific categories are more likely to experience this issue. The American Academy of Ophthalmology (AAO) states that the following groups are at particularly high risk of glaucoma:
- Anyone age 40 or older
- Those with a family history of glaucoma
- Those who are nearsighted or farsighted
- Those with other chronic eye conditions
- Anyone who has injured their eyes in the past
- Those with high blood pressure
- Those with diabetes
- Those with poor blood circulation
If you fit into any of these categories, then you are at a heightened risk of developing glaucoma. Monitoring this is worthwhile and can have a real impact on your day-to-day life if you do not stay on top of it.
What to Expect During a Tonometry Test
 Patients often find themselves anxious about any kind of medical examination that they may be subjected to. In many ways, this is completely understandable.
Patients often find themselves anxious about any kind of medical examination that they may be subjected to. In many ways, this is completely understandable.
They do not take these tests every day. They may not know how the test works when they first arrive. Luckily, a tonometry test typically concludes within just seconds.
You may need to take a tonometry test several times to get a result, depending on the testing method. Some optometrists like to take the average results from several tests. They do this before giving a conclusion. They perform this action to better ensure the quality of the data they are looking at.
After all, they would rather know with a higher degree of certainty that their test results are accurate. This means getting multiple samples of the data before drawing a conclusion.
Patients need not worry excessively about undergoing these tests. Although they may experience a momentary discomfort when the puff of air contacts their eye, it’s fleeting. Typically, the entire process concludes in merely a few seconds. The readings will be available to them right away.
What Happens After the Test?
Once the test has concluded, the results should be available to the Ophthalmologist within mere seconds. He or she will review that data and then present their findings to the patient.
If the patient has received anesthetic drops for testing, they should not touch or rub their eyes. Waiting until the drops wear off is important.
The purpose of the drops is to keep your eyes numb while the testing procedure is occurring. However, that numbness can make it easier to injure your eyes. If the patient rubs their eyes, they may not feel how hard they are rubbing.
How to Interpret the Tonometry test results
 The only people who are qualified to fully interpret tonometry test results are optometrists. They have spent many years in medical school. They learned how to read test results like this one. We should trust their interpretation of these results above all else.
The only people who are qualified to fully interpret tonometry test results are optometrists. They have spent many years in medical school. They learned how to read test results like this one. We should trust their interpretation of these results above all else.
That said, there are some general guidelines that even a layperson can think about when considering the results of their test. Healthline.com explains:
According to the Glaucoma Research Foundation, the normal eye pressure range is 12 to 22 mm Hg. The measurement “mm Hg” means “millimeters of mercury,” which are the units used to record eye pressure. If your test comes back with a pressure reading that’s higher than 20 mm Hg, you may have glaucoma or pre-glaucoma.
They explain that high pressure in the eyes is one possible sign of glaucoma. Having a doctor examine you before deciding that you have glaucoma is important. There may be other reasons for the high pressure in your eyes. Letting the professionals figure this out is best.
If a doctor finds that their patient has glaucoma, they will quickly start discussing treatment options. Once again, the treatment options available to a given patient will vary depending on the specifics of their case. Remember that when considering what kind of recommendations people are likely to make, it is important.
Should a Patient Drive Following a Tonometry Test?
Among the most common questions brought up by patients who have undergone a tonometry test is if they should drive following the test. Some procedures at an optometrist’s office can prevent a patient from driving home safely afterward. Therefore, it is a reasonable question to ask.
The answer to this question depends on several factors related to a patient’s tonometry test. Among the most important factors is if eye dilation was necessary for a given patient’s test. Patients who have had their eyes dilated should bring someone along with them who can safely drive them home following the procedure. Driving themselves in this scenario is unsafe for them.
Dilation of one’s eyes causes light sensitivity. This renders reading items at a close range challenging. It can also make it tough to see important parts of the road while driving. Whenever an eye doctor dilates your eyes during an eye exam, you should bring someone to drive you home.
Early Detection of Glaucoma is the Best Way to Start Treating
Some patients avoid visiting their optometrist. They fear the puff of air in their eye or other tests. This small amount of discomfort is worth it. It can make a significant difference in finding glaucoma early.
As we mentioned at the top, glaucoma is an increasingly common disease. The most effective approach is early detection. Initiate a conversation with your physician about potential treatment strategies at your earliest convenience.
A simple tonometry test can detect the high pressure inside the eye that often results from glaucoma. Knowing your situation and whether you need to take steps to treat your glaucoma is much better. Staying informed is better than ignoring these important facts.
Your eye care specialist can recommend treatments that can help you take care of the high pressure in your eyes. This can ease some of the tension that you might have been feeling about all this.
It can also help you feel better about your eye health in general. In the end, it can lead to better results. You would not have appreciated these if you had not visited your doctor.
Handheld tonometers improve ophthalmic care by providing accurate and mobile options for glaucoma detection and tracking intraocular pressure.
At-Home Tests and Other Developments
Ultimately, we aim to leave you with a hopeful message. Many exciting developments have emerged in the realm of tonometry tests in recent years.
One option is the at-home tonometry tests. These tests are now available for people who need to check their eye pressure regularly. A doctor can guide the use of these devices. They provide more reliable and consistent data over longer periods.
Patients using these devices can give their doctors important information about their eye pressure levels at any time. This can help a doctor understand the average pressure readings for a patient. It shows how worried they should be about the possible development of glaucoma. This data can also help add to the research and information about glaucoma in the general population.
Researchers know a lot about glaucoma, but the world continues to learn even more with each passing year. Both patients and doctors should feel excited that researchers are conducting more studies on this important topic.
The more we learn, the better our treatments will become.This is all thanks to tonometry devices. They provide safe and reliable results quickly. Keep an eye out for how they will continue to improve.
Matthew Strachovsky, M.D.
Dr. Strachovsky's undergraduate training began in Boston, Massachusetts at Boston University and was completed at Stony Brook University in Long Island, NY. There he graduated Summa Cum Laude, obtaining a Bachelor of Science degree in Biology with special recognition for academic achievement.
He continued his education at Stony Brook School of Medicine and graduated with the additional designation of the "MD with Recognition" program. He worked as an intern in Internal Medicine at Winthrop University Hospital in NY and pursued a residency at Stony Brook University Hospital in Ophthalmology acting as Chief Resident in his final year. He completed his fellowship training in Vitreoretinal disease with a major emphasis on the diagnosis and management of retinal vascular diseases under the direction of Dr. Michael O'Brien at Koch Eye Associates in Rhode Island.
Dr. Strachovsky has presented research at the annual Association for Vision and Research in Ophthalmology meeting and published articles in journals including, Investigative Ophthalmology and Visual Science and The Journal of Neuro-ophthalmology.
Dr. Strachovsky's professional interests include the management of Age-Related Macular Degeneration and diabetic eye disease. He is Board Certified in Ophthalmology and a member of the American Academy of Ophthalmology, American Society of Retina Specialists, Young Ophthalmologist Network, and Leading Physicians of the World.
" I believe that the physician/patient relationship is more important than ever. Being an Ophthalmologist allows me to help patients and build a foundation of trust, knowledge, and professionalism when it comes to eye care".