Table of Contents
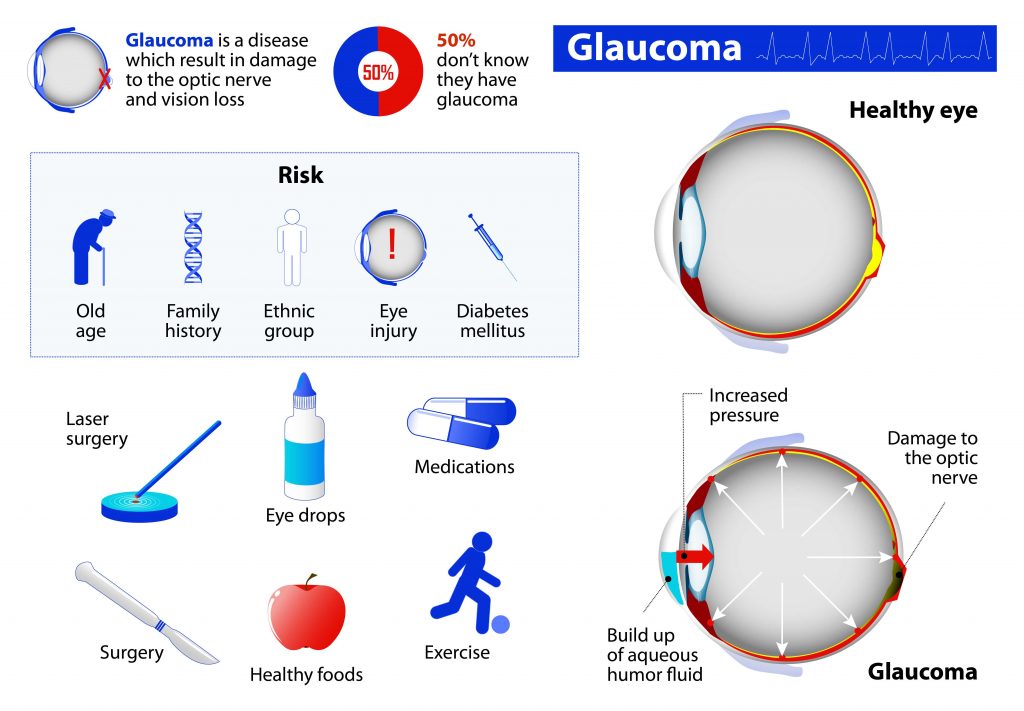
Glaucoma is caused by the buildup of pressure inside the eye, damaging the nerve connecting the eye to the brain. However, the damage on the optic nerve is not caused by one case of Glaucoma but rather a group of eye conditions known to cause blindness. The disease has been established to affect adults more than the younger generation.
The condition had to detect because during onset, it doesn’t present with any symptoms but grows gradually, and one will only know about it when it is in its advanced stages. The high pressure on the eyes is due to the buildup of aqueous humor, a fluid that usually flows inside a person’s eye.
How Glaucoma Testing Equipment helps patients in COVID-19 Pandemic.
While inside the eye, the fluid drained out via the trabecular meshwork at an angle where the iris and cornea meet, and here is where the problem develops. At times, the drainage system fails to work appropriately, thus retaining the fluid increasing pressure on the eyes. Other times the eye overproduces the fluid.
The ability of your eye to either retain or drain the intraocular fluid is dependent on the type of Glaucoma that one has. So as eye pressure keeps building, it pushes against the optic nerves, which permanently damages the nerve fibers leading to blindness.
Glaucoma is also caused by poor blood flow, Optic Nerve Damage
Glaucoma has also been determined to develop when the eye’s internal pressure is normal, also known as “Normal-Tension Glaucoma.” individuals who experience this problem have optic nerves that are pressure sensitive and are, therefore, susceptible to irreversible damage. The above condition under different circumstances would be considered normal.
Important to note is that people who have high intraocular pressure, also known as ocular hypertension, might never develop Glaucoma. Little evidence exists on the cause of normal-tension Glaucoma; the theory that exists, therefore, suggests that a reduction in the blood that flows to the optic nerve may be the primary cause.
Therefore, the decrease is believed to be a result of the narrowing of the blood vessels necessary for nourishing the optic nerve or due to the constriction of blood vessels. Another major cause of Glaucoma, according to researchers, is the buildup of protein (beta-amyloid) in brain tissue and the eye’s Retina.
The above has also been determined to cause Alzheimer’s. Still, it is clear that even though a person may accumulate beta-amyloid proteins, it does not directly mean that the other person will have Alzheimer’s or Glaucoma.
 How to prevent Glaucoma
How to prevent Glaucoma
Glaucoma is an eye condition that needs to be kept at bay at all costs because of its ability to cause vision loss. Glaucoma is not restricted to older adults. Therefore, anyone can contract it, especially those in the below category.
- Individuals who are 40 years old and above
- People suffering from high blood pressure
- Individuals with diabetes
- Those who have a history of the disease in their family
- And people of the Hispanic or African American descent
With the above in mind, people can observe the below measures, which will help prevent Glaucoma. The first step is to understand the history of your family, and if anyone along your lineage developed the disease, and if the condition was present, then you should expose yourself to frequent screenings.
Regular and moderate exercises have also been determined to reduce the chances of developing Glaucoma, as they help reduce eye pressure. Therefore, your doctor is better positioned to propose the best exercise routines that you can adopt.
Protection as always is better than cure, and you, therefore, need to protect your eyes at all costs because if by any chance you suffer eye damage, then chances of developing Glaucoma are very high. Also, individuals who use high-power tools or play high-speed racket sports will be safe if they use eye protection.
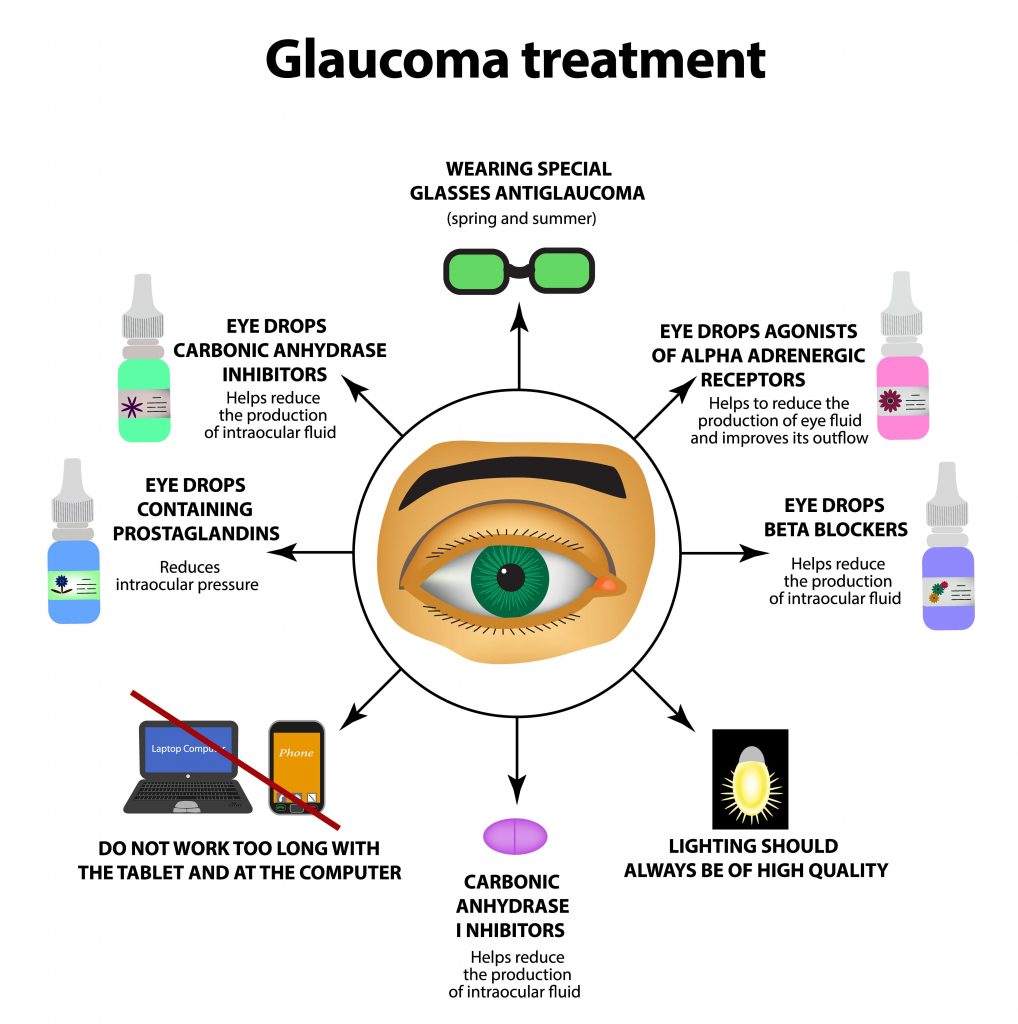
Doctors do prescribe Glaucoma eye drops that help limit the chances of developing Glaucoma, so if your doctor prescribed the eye drops, then be sure to use them as defined as they will help obliterate the chances of developing the condition if you don’t have any severe symptoms yet.
Dilated eye examinations are also necessary as they help detect the disease while still in its early stages. Individuals under 40 could, therefore, have eye checkups every five years to ten years, and for those who are between 40 and 54 years old, then the testing period shortens to two or four years. And older adults between the ages of 55 and 64 can have their checkups between one to three years.
Individuals older than 65 will have to take their checkups at least one to two years. There are also other do-it-yourself preventive measures that you can incorporate into your daily lifestyle, which will help lower your chances of developing Glaucoma.
You should, therefore, exercise daily. You could swim, walk, or do manual jobs in the yard. And when there is too much sun outside, protect your eyes by wearing a hat or sunglasses anytime outdoors. Evidence suggests that high amounts of caffeine intake could increase eye pressure, quit or don’t smoke, and maintain a healthy weight; your blood pressure should also be held at a reasonable level.
Foods that can help enhance eye health.
When it comes to foods that can help boost your eye health, then you have a broad spectrum, from foods rich with vitamin D, such as egg yolks, cereals, and fortified milk, to those containing vitamin A, such as sweet potatoes, mangoes, carrots, and liver. Fruits and vegetables are also a good source of food but ensure to get the ones that are dark green and yellow.
Foods rich in Zinc such as poultry, red meat, and nuts are also nutritious for your eye, and foods packed with omega-three fatty acids such as flax seeds, wild salmon, and chia seeds, among others, are also helpful.
As we have determined above, Glaucoma does not come with any bells or whistles, and you will have to implement the various preventive measures suggested above. However, if you all of a sudden experience severe headache, blurred vision, or pain in the eyes, then you will have to visit an eye doctor, “an Ophthalmologist with Glaucoma Testing Equipment, immediately.”
Guidelines for ophthalmologists and staff when checking Glaucoma patients in COVID-19 Pandemic
- Non-contact dispensers will be provided at the hospital’s entrance, where all patients and the accompanying persons will be asked to wash or disinfect their hands.
- Each patient will then be asked if they have a cold, fever, cough, flu symptoms, or conjunctivitis. If they present any of the above symptoms, they will be invited to the hospital’s outpatient service and not the emergency room.
- Patients are then advised to have their masks on the entire time they are in the office and during the examinations. The masks are to cover the mouth and the nose adequately. The idea behind putting on a mask is to prevent droplets emitted from speaking, breathing, and sneezing from reaching the other person. The move above is to reduce the risk of transmitting the virus.
- Patients should observe a distance of one meter or more and restrain themselves from touching the various parts of their faces: the nose, mouth, and eyes, including multiple surfaces within the office.
- No physical contact is allowed between the patients and the staff. Kisses and hugs should also be avoided.
- Dispensers of detergent-sterilizing substances to be used for cleaning the hands should be placed inside the medical practitioner’s offices, and patients encouraged to use them as frequently as possible.
- Information derived from the non-contact temperature measurements cannot be entirely relied on and can only screen patients in the office.
Preventive measures for staff who get into contact with the patients.
- The team is always advised to have their masks on and try as much as they can not to touch the masks. During removal, they should begin by first removing the rubber bands at the back of their ears.
- Staff members are advised to wear protective glasses for their safety during the clinical examinations and while at the office.
- Examinations should be carried out with minimal contact between doctor and patient. Still, if communication is necessary, the healthcare professional is advised to wear protective gloves that are to be replaced after each patient. And a disinfection procedure of the hands should follow after removal of the masks.
- All surfaces and instruments that come into contact with the patient should be disinfected, and a procedure is done in-between visits to protect patients that will come after.
- Clean the surfaces, switches and handles, and any object that might have come into contact with the hands and faces of the patients and staff. The keyboard, mouse, and telephone should all be cleaned with detergent and sterilizing solution from time to time. Disposable gloves will be used at this point, and the hands will be disinfected immediately afterward.
- The chin guards should always be cleaned, the borders of instruments and test glasses that patients came into contact with, and all parts of the instruments touched by the patients. The above procedure is to be done at the beginning of the examination and in the patient’s presence.
- All the instruments that come into contact with the patient’s eyes should be cleaned and sterilized. Medical practitioners should use contact tonometers if possible and avoid the use of contact lenses, such as the 3-mirror or the gonioscopy.
- Volk-type lenses or single-use contact lenses should, therefore, be used if possible. Touching of patients’ eyelids, nose, and mouth is not encouraged, and if it is a must, then gloves should be used. The conjunctiva offers safe passage for the COVID 19 virus to enter the body, so a person’s own eyes and face should not be touched.
- Multi-dose eye drops should not be used as they can be a source of contamination when they touch the eyelids and the conjunctiva of patients and via the non-sterilized hands of the healthcare professionals.
- Therefore, if possible, healthcare professionals should use single-dose products, and that is if they need to use multiple doses. Medical professionals should also avoid contact with the regulator or their hands with parts of their patient’s face.
- Medical practitioners should avoid handling the patient’s contact lenses or even applying them, and they should also prevent non-contact tonometry (air-puff tonometry). Using the latter on patients found to be having COVID -19 might produce a high amount of virus-loaded aerosol in the local area, thus encouraging the spread of the virus.
Here are the Top 10 Glaucoma Testing Equipment for An Ophthalmologist
1. ZEISS CIRRUS 6000 from Zeiss
The ZEISS CIRRUS 6000 is a high-performance Glaucoma testing machine that enables medical practitioners to get up to 100,000 scans per second; the unit offers a larger field of view of up to 12mm in a single scan, thus enabling diagnosis of the existing condition. ZEISS CIRRUS also captures high definition OCT and OCT Angiography scans; medics will, therefore, be able to reveal the finer microvascular details of the Retina, thus gaining more insight into their patient’s condition.
Clinicians can also access extensive clinically validated applications for Glaucoma, Retina, and the anterior segment; the above features enable the clinicians to carry out precise analysis and make smarter decisions when dealing with a variety of clinical conditions and patient types.
2. Plex Elite 9000 from Zeiss
Plex Elite 9000 offers advanced OCT imaging technology that enables retina and glaucoma researchers more in-depth insight into the structural and microvascular clarity of the eye. Clinicians will, therefore, be able to access faster and deeper images with higher resolution. The unit also comes equipped with a new dual-speed PLEX Elite that elevates ophthalmic imaging and clinical research.
The Plex Elite 9000 gives the clinicians a chance to study the new mechanisms of micro and neovascularization of the posterior segment from the vitreous to the sclera. Also enabled are the capabilities of exploring the progression of the retinal and choroidal pathology, for example, the CNV.
3. Nidek Mirante
The Nidek Mirante offers clinicians the ultimate multimodal imaging platform with an ultra-wide field of view. Here we discuss the entire 163° field of view that enables a detailed evaluation of pathologies from the fovea to the extreme periphery. The enabled 4,096 x 4,096-pixel imaging can capture every detail of the Retina and choroid.
Clinicians can also zoom in for higher magnification and clear visualization of the changes in pathology and resolution of the finer details of the capillaries. Furthermore, the imaging platform has also been equipped with three separate RGB detectors that can simultaneously scan different depths of the Retina by utilizing the red, green, and blue wavelengths.
4. Maestro2 from Topcon
The Maestro 2 is a fully automated OCT/FUNDUS camera that has been equipped with an OCT Angiography complete with data management. Clinicians can use the unit to access the hood report that gives information on the structure and analysis of Glaucoma. Even more important is that the OCT camera features a 360° rotating intuitive touch screen.
Clinical utilities have also been loaded to the Maestro, such as the IMAGE net six capture software that enables dynamic viewing of the OCT and imaging data. The unit has also been equipped with a new follow-up scan feature, which can scan the exact location of each patient, thus providing reliable follow-up information for each patient visit and tracking of diseases over time.
5. Optovue Avanti
Optovue Avanti is a comprehensive wide-field OCT imaging that calculates the IOL power in your post; it also enables visualization of peripheral pathology with Avanti’s 3D wide-field cube. Clinicians will get new views of the Retina because the Optovue Avanti provides further information on the structures located outside the traditional 6×6 mm cube, which separates the Retina into distinct layers to enable detailed assessment.
Views of the vitreous and the deep choroid have also been provided, and clinicians will also be able to monitor change over time. Avanti, therefore, offers extensive information that enables clinicians to tailor their approach towards treatment and consequently personalize patient care.
6. CIRRUS PHOTO 600 from Zeiss
The Zeiss Cirrus photo is available in two models, the Zeiss photo 600 and 800; the above offers many insights to enable the clinicians to come up with a whole retina and posterior segment care. The images provided by Zeiss Cirrus give a more comprehensive diagnostic insight.
Besides, each modality is a premier quality diagnostic instrument that, when combined, the clinician will be able to characterize and examine a patient’s condition more comprehensively. Other features that will be made available to the clinicians include high-resolution angiographies and the single short fundus autofluorescence. Zeiss optics also enable visualization of the findings with high-resolution clarity.
7. Haag-Streit at900
Tonosafe is a disposable measuring prism designed to help reduce the risk of infection between patients. The measuring prisms are reusable and distinguished by their optical and mechanical performance, allowing fast and reliable measurements in daily practice.
The units are made by experienced workers and are quality checked for tight optical quality, durability, and consistent measurement results. And to carry out a successful disinfection routine, clinicians have been provided with the Haag-Streit Desinset.
Clinicians will, therefore, be able to carry out examinations without taking too much time or compromising the quality of the original Goldmann quality.
8. Topcon ct 800
The ct 800 is a computerized tonometer that offers smooth operation and allows comfortable use. The computerized tonometer has been equipped with a wide 8.5-inch touch screen panel with clear and very easy-to-read icons, designed to allow the complete operator control of the unit when measuring.
The incorporated soft air puffs control the optimum amount of air required for every measurement, and that is for each of the eyes, thus less stress on the eye; therefore, patients can experience less stress on their eyes. The unit can also calculate the adjusted Tono value from the measure IOP to manually inputting the corneal thickness value that other devices have measured.
9. Topcon ct-1p
The Topcon ct-1p features a compact design thus can be installed in various positions in the examination room. The Topcon has been equipped with comfort and safety features such as the optical head and headrest and the stable IOP measurement complete with soft air-puff. Clinicians using the units for measurements could use the manual, and immediately it detects the pupil position. The movement will retain alignment, and you will have to press the start button.
The incorporated additional measurement mode helps save time, thus preventing extra work and inconvenience. The control panel features and touch screen control panel, and the incorporated CT-1P automatically takes measurements of the left and the right eye.
10. Henson 9000
The Henson 9000 has been equipped with an intelligent supra for detection, utilizing the latest research to incorporate 24-2 and 10-2 patterns. Clinicians have also been equipped with all the tools they might need to enable cross-compatibility between smart supra and Zata and detailed progression analysis.
What’s more, is that the compact design allows easy positioning in space-constrained environments. Both the patient and the clinician will also be able to enjoy flexibility because of the equipped smart supra multiple stimulus tests that minimize patient response errors and speed up the test times and make it even more helpful. The smart stimulus has also been provided.
Conclusion
Glaucoma is a severe eye infection that may render one permanently blind; therefore, ophthalmologists must treat individuals suffering from the disease. However, with the world now on lockdown because of the COVID 19 pandemic, personal hygiene is the best-proposed method of prevention to help prevent contracting or transfer of the disease.
Doctors are, therefore, at risk of contracting COVID 19 when treating patients who have been infected with the disease; the reason we have provided you with the updated protective measures complete with some of the disposable Glaucoma Testing Equipment, which reduce chances of infection.
Matthew Strachovsky, M.D.
Dr. Strachovsky's undergraduate training began in Boston, Massachusetts at Boston University and was completed at Stony Brook University in Long Island, NY. There he graduated Summa Cum Laude, obtaining a Bachelor of Science degree in Biology with special recognition for academic achievement.
He continued his education at Stony Brook School of Medicine and graduated with the additional designation of the "MD with Recognition" program. He worked as an intern in Internal Medicine at Winthrop University Hospital in NY and pursued a residency at Stony Brook University Hospital in Ophthalmology acting as Chief Resident in his final year. He completed his fellowship training in Vitreoretinal disease with a major emphasis on the diagnosis and management of retinal vascular diseases under the direction of Dr. Michael O'Brien at Koch Eye Associates in Rhode Island.
Dr. Strachovsky has presented research at the annual Association for Vision and Research in Ophthalmology meeting and published articles in journals including, Investigative Ophthalmology and Visual Science and The Journal of Neuro-ophthalmology.
Dr. Strachovsky's professional interests include the management of Age-Related Macular Degeneration and diabetic eye disease. He is Board Certified in Ophthalmology and a member of the American Academy of Ophthalmology, American Society of Retina Specialists, Young Ophthalmologist Network, and Leading Physicians of the World.
" I believe that the physician/patient relationship is more important than ever. Being an Ophthalmologist allows me to help patients and build a foundation of trust, knowledge, and professionalism when it comes to eye care".