Table of Contents
Around 3 million Americans have glaucoma, and it’s the second leading cause of blindness worldwide. This alarming statistic underscores the critical importance of intraocular pressure measurement (IOP testing) in eye care.
Eye care professionals must have the best monitoring tools to manage eye pressure. Handheld tonometers, which offer portable tonometers that combine precision with convenience, are leading the revolution in this category.
Handheld tonometers improve eye care by providing accurate and portable solutions for glaucoma screening and monitoring eye pressure.
Understanding Intraocular Pressure (IOP) and Its Significance
Intraocular pressure (IOP) refers to the fluid pressure inside the eye. Maintaining a healthy IOP is crucial for the overall health of the eye.
Elevated IOP can lead to glaucoma, a condition that damages the optic nerve and can result in irreversible blindness. Regular IOP testing is vital for early detection and management of glaucoma and other eye conditions.
Tonometry is the method used to measure IOP. While effective, traditional tonometry devices often require stationary equipment and specialized settings.
Portable tonometry devices, like handheld tonometers, have made testing eye pressure more convenient for eye care professionals. These devices can easily be carried to various locations for testing, and thanks to them, eye care professionals can now test eye pressure in different settings. Portable tonometry devices offer flexibility and accessibility without compromising accuracy.
What Is a Handheld Tonometer?

A handheld tonometer is a portable device that measures the eye’s intraocular pressure. Unlike older tabletop tonometers, handheld tonometers are small, light, and simple, perfect for quick eye exams. These devices have advanced technology that ensures accurate readings, even in non-clinical settings.
Doctors widely use handheld tonometers in glaucoma screening, where early detection of elevated IOP is critical. These devices are also invaluable in situations where transporting patients to a clinical setting is challenging, such as:
- In rural areas
- During home visits
The portability and accuracy of these devices make them an essential tool in modern eye care.
Advantages of Handheld Tonometers
The benefits of handheld tonometers extend beyond their portability. These devices offer several advantages, making them a preferred choice for eye care professionals.
Portability
One of the standout features of handheld tonometers is their portability. These small and light devices are easy to carry. This makes them perfect for eye care professionals. They can test eye pressure in different locations.
Handheld tonometers provide easy access to quality eye care in clinics, hospitals, and patients’ homes. This is helpful in places with limited eye care facilities, like remote or rural areas.
Portable eye care devices, like handheld tonometers, make eye care services more accessible to access and reach for patients.
Accuracy
Despite their small size, handheld tonometers maintain accuracy. These devices are engineered to provide precise and reliable IOP measurements. This is crucial for effective glaucoma screening and ongoing eye pressure monitoring.
Technology advancements have allowed portable tonometers to match the accuracy of their larger, stationary counterparts. They are an indispensable tool in routine check-ups and specialized care.
It’s a level of accuracy that ensures the following:
- Eye care professionals can make informed decisions about a patient’s treatment plan
- Reduced risk of misdiagnosis
- Eye pressure monitoring is consistent and dependable
Ease of Use
Another significant advantage of handheld tonometers is their user-friendly design. These devices have intuitive interfaces that require minimal training, making them accessible to a wide range of users, including:
- Technicians
- Nurses
- Other healthcare staff
This device is easy to use, which is helpful in busy practices where time is limited and many people need it. Handheld tonometers have easy controls and clear instructions, making it simple for inexperienced users to get accurate readings quickly. This improves workflow and patient care.
Patient Comfort
Patient comfort is crucial during IOP testing; handheld tonometers excel in this area. Traditional tonometry devices can be uncomfortable, especially when they require direct contact with the eye.
In contrast, many handheld tonometers use non-invasive techniques that minimize discomfort. It’s a benefit that’s particularly important for sensitive populations, such as:
- Children
- Seniors
- Those with anxiety about eye exams
By enhancing the patient experience, handheld tonometers encourage more frequent testing and better compliance with recommended screening schedules.
Versatility
The versatility of handheld tonometers is unmatched. These devices, including regular eye exams, are easy to use in various medical situations. They are also helpful in emergencies that require quick and accurate eye pressure measurements.
Handheld tonometers can be used in many locations, such as clinics and mobile units, making them adaptable to different patient needs and environments.
Their ability to perform reliably across different contexts makes them a valuable addition to any eye care professional’s toolkit. It guarantees that comprehensive eye care is always possible, regardless of the setting.
Guide to Choosing the Right-Handheld Tonometer
 Selecting the right handheld tonometer for your practice involves considering several factors. Here’s a guide to help eye care professionals make an informed decision.
Selecting the right handheld tonometer for your practice involves considering several factors. Here’s a guide to help eye care professionals make an informed decision.
Accuracy and Precision
The primary function of a handheld tonometer is to provide accurate IOP measurements. When choosing a device, ensure that someone has tested and validated it against gold-standard tonometers. Look for devices that offer consistent readings across various patient populations and conditions.
Ease of Use
A user-friendly interface is crucial, especially in fast-paced clinical environments. Consider devices that offer:
- Simple controls
- Clear displays
- Straightforward instructions
Some handheld tonometers also come with automated features that reduce the risk of user error.
Cost and Value
While cost is an important consideration, it should be weighed against the device’s value to the practice. Handheld tonometers that offer advanced features, durability, and reliable support services may justify a higher initial investment. Consider the long-term benefits of the device, including:
- Its impact on patient outcomes
- Practice efficiency
Clinical Needs
Different handheld tonometers are suitable for various clinical settings. Some are better suited for pediatric patients, while others are ideal for elderly patients with mobility issues. Please consider the specific needs of your patient population when choosing a device.
Brand and Support
Reputable brands like Nava Ophthalmic offer reliable handheld tonometers with robust customer support. Choose a device from a manufacturer known for quality products and responsive service.
Comparing Types of Handheld Tonometers
Several types of handheld tonometers are available. Look at each and its advantages and use cases:
Applanation Tonometers
These devices measure IOP by flattening a small area of the cornea. They provide high accuracy and often serve as the gold standard in tonometry. However, they require contact with the cornea, which may cause discomfort in some patients.
Rebound Tonometers
Rebound tonometer devices measure IOP by bouncing a small probe off the cornea. They are non-invasive and generally more comfortable for patients, making them popular as portable eye care devices.
Indentation Tonometers
Indentation tonometers measure IOP by indenting the cornea with a small plunger. They are less commonly used today but can be helpful in specific clinical situations.
How to Use a Handheld Tonometer

Using a handheld tonometer is straightforward. However, following the correct procedures is essential for accurate intraocular pressure (IOP) measurements. Proper technique guarantees reliable results and enhances patient comfort and safety.
Here’s a detailed step-by-step guide on using a handheld tonometer.
1. Patient Preparation
You can begin by using a headrest to ensure the patient is seated comfortably with their head well-supported. A stable head position is crucial for obtaining accurate readings.
Instruct the patient to look straight ahead and remain as still as possible during the test. Tell the patient about the procedure in advance to reduce anxiety and movement and ensure more accurate IOP test results.
- Comfort is Key: A relaxed patient is less likely to move during the test, which is vital for accurate measurements
- Clear Instructions: Guide the patient through the process so they know what to expect
2. Device Preparation
Preparing the device is simple. Before using the handheld tonometer, do the following:
- Turn on the device
- Ensure that it is functioning correctly
- Choose the correct settings for the patient, like adjusting sensitivity or calibration if needed.
It is also essential to verify the following:
- The probe or sensor is clean
- Properly aligned
- Free of any debris that could interfere with the reading
For portable tonometers with disposable probes, permanently attach a new, clean probe before each use to avoid spreading germs.
- Check Calibration: Calibrate the tonometer according to the manufacturer’s guidelines to maintain accuracy
- Ensure Cleanliness: Always use a clean, sterile probe to prevent infections and ensure the reliability of the tonometry device
3. Measurement Procedure
Please position the handheld tonometer near the patient’s eye, following the manufacturer’s instructions to avoid causing any discomfort. You should bring the device close to the cornea while maintaining a steady hand to prevent sudden movements.
The handheld tonometer will automatically measure the intraocular pressure and display the results on its screen. To obtain an accurate reading, you must ensure the tonometer aligns with the cornea.
Depending on the type of tonometer, the device may measure the IOP using applanation, rebound, or indentation techniques.
- Steady Handling: Hold the device steadily to avoid any sudden movements that could affect the accuracy of the reading
- Proper Alignment: Ensure the tonometer is aligned with the cornea for an accurate intraocular pressure measurement
4. Recording and Analysis
After the IOP is measured, record the readings immediately in the patient’s medical record. Accurate records are important for monitoring changes in eye pressure over time, especially for managing conditions like glaucoma.
Could you compare the current results to past ones? This will help you find any critical changes. These changes could indicate that an eye condition is worsening or that treatment must be adjusted.
- Accurate Documentation: Ensure that the IOP readings are recorded in the patient’s file for future reference
- Trend Analysis: Compare new readings with historical data to monitor any trends in eye pressure that could indicate worsening conditions
5. Post-Measurement Care
Once the measurement is complete, take care of the handheld tonometer so it remains in good working condition. It is essential to clean a contact tonometer as directed by the manufacturer. This helps avoid contamination and ensures accurate readings in the future.
For devices with disposable parts, such as single-use probes, dispose of them and replace them as required.
- Thorough Cleaning: Clean the tonometer’s probe or sensor according to the manufacturer’s instructions, especially if it comes into direct contact with the eye
- Preventive Maintenance: Check and maintain the device to ensure its longevity and consistent performance
Please follow these steps to ensure handheld tonometers provide accurate and reliable IOP tests. These tests are crucial for effective glaucoma screening and monitoring of eye pressure. Using portable eye care devices correctly improves accuracy in diagnosis and ensures patient comfort and safety during procedures.
The Role of Handheld Tonometers in Glaucoma Screening
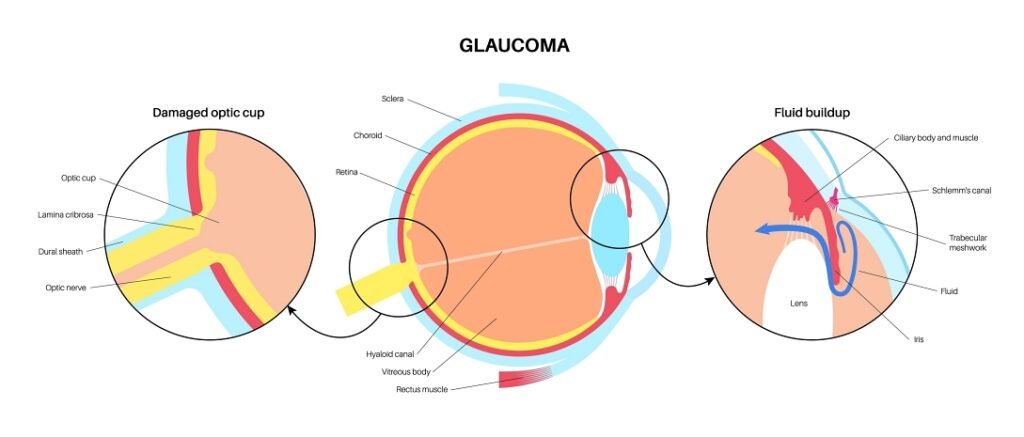
Glaucoma is a silent disease, often progressing without noticeable symptoms until significant vision loss has occurred. Regular IOP testing is the most effective way to detect glaucoma early.
Handheld tonometers are important for glaucoma screening. They are used in community health centers, mobile clinics, and for home care.
Portable tonometers are particularly beneficial for screening high-risk populations, including:
- Seniors
- African Americans
- Those with a family history of glaucoma
These devices’ ease of use and comfort encourage more frequent testing, leading to earlier diagnosis and treatment.
Advancements in Handheld Tonometry Devices
The field of tonometry has seen significant advancements, with handheld tonometers at the forefront of these innovations. Modern handheld tonometers are equipped with features that enhance the following:
- Accuracy
- Ease of use
- Patient comfort
Some of the latest advancements include these features.
Wireless Connectivity
Many handheld tonometers now offer wireless connectivity, allowing for seamless integration with electronic medical records (EMRs). This feature streamlines the documentation process and ensures accurate record-keeping.
Automated Measurement
Some devices have automated measurement capabilities. This feature reduces the risk of human error and ensures consistent results.
Multi-Functionality
Certain handheld tonometers perform multiple tests, such as measuring corneal thickness and IOP. This multi-functionality enhances the device’s utility and provides comprehensive eye care in a single tool.
Enhanced Portability
Newer models are even more compact and lightweight, making them easier to carry and use in various settings. Despite their small size, these devices maintain accuracy and reliability.
Choosing the Right-Handheld Tonometer for Eye Care Professionals

When selecting a handheld tonometer, it’s essential to consider the specific needs of your practice and patients. Here are some key factors to keep in mind.
Patient Population
Could you consider the demographics of your patient population? For instance, pediatric patients may require a noninvasive, gentle device, such as a rebound tonometer, which is more comfortable for children.
Older patients with cataracts or dry eyes may benefit from using a handheld tonometer. This device can reduce discomfort and provide accurate readings, even on uneven eye surfaces.
Clinical Setting
The environment in which the handheld tonometer will be used is crucial. A lightweight, battery-operated device with long-lasting power is ideal for mobile clinics or home visits. A model that works well with other tools and medical records is better for busy hospitals or clinics.
Ease of Disinfection
With the increasing emphasis on infection control, the ability to disinfect the tonometer between uses is vital. Designers create some devices with smooth surfaces and detachable parts that users can easily clean. This ensures patient safety and reduces the risk of cross-contamination.
Support and Training
Even the most advanced handheld tonometer is only as good as the support and training provided by the manufacturer. Make sure the brand you choose offers the following:
- Comprehensive training materials
- User manuals
- Responsive customer service
Brands like Nava Ophthalmic provide excellent post-purchase support so eye care professionals can confidently use their devices.
Integration of Handheld Tonometers in Routine Eye Care
 Adopting handheld tonometers in routine eye care has shifted how intraocular pressure is monitored. Eye care professionals are increasingly integrating these devices into their regular patient assessments. They recognize their value in enhancing patient care and improving diagnostic accuracy.
Adopting handheld tonometers in routine eye care has shifted how intraocular pressure is monitored. Eye care professionals are increasingly integrating these devices into their regular patient assessments. They recognize their value in enhancing patient care and improving diagnostic accuracy.
Routine Eye Exams
Handheld tonometers are now used during routine eye exams. They allow for quick and efficient IOP testing. Their ease of use and minimal discomfort make them ideal in busy clinics with high patient throughput.
Specialty Clinics
Handheld tonometers are crucial for monitoring disease progression and treatment efficacy in specialty clinics focusing on glaucoma or pediatric ophthalmology. Their portability allows for consistent monitoring in various settings, ensuring patients receive timely care.
Telemedicine and Remote Care
The rise of telemedicine has further highlighted the need for portable diagnostic tools. Medical professionals can use handheld tonometers during remote consultations to provide accurate IOP measurements, which they can discuss with patients via video calls. This capability is particularly beneficial for patients in rural or underserved areas.
The Future of Handheld Tonometry Devices
As technology continues evolving, the future of handheld tonometry devices looks promising. Innovations in sensor technology, artificial intelligence, and data integration further enhance these devices’ capabilities, making them even more indispensable in eye care.
AI-Enhanced Diagnostics
Future handheld tonometers may incorporate artificial intelligence to assist in interpreting IOP readings. They may provide real-time analysis and suggest potential diagnoses. This advancement could further reduce the margin for error and assist practitioners in making informed decisions.
Integration With Wearables
There is potential for handheld tonometers to be integrated with wearable technology. This would allow for continuous monitoring of intraocular pressure, which could be helpful in patients with fluctuating IOP and provide valuable data-tailored treatment plans.
Improved Accessibility
As these devices become more affordable and available, specialists, general practitioners, and optometrists will likely adopt handheld tonometers. It will lead to more widespread glaucoma screening and eye pressure monitoring.
Practical Tips for Maintaining a Handheld Tonometer

Proper maintenance protocols are essential to ensuring the longevity and accuracy of handheld tonometers. Here are some practical tips.
Regular Calibration
Even the most advanced tonometers require regular calibration to maintain accuracy. Follow the manufacturer’s guidelines for calibration frequency and procedures.
Cleaning and Disinfection
After each use, clean the device according to the manufacturer’s instructions. Pay special attention to parts that come into contact with patients, and use only approved disinfectants.
Battery Maintenance
Be sure the device’s battery is charged and functioning properly. Change batteries when necessary and turn off the device when not in use to save battery life.
Software Updates
If your tonometer includes software, could you update it to include the latest versions? These updates often improve accuracy and functionality.
Checking for and installing updates can also enhance the device’s user interface, making operating easier. Additionally, updates may introduce new features that further improve the efficiency and effectiveness of intraocular pressure measurement (IOP testing).
Storage Conditions
Store the handheld tonometer in a clean, dry environment to prevent damage from moisture or dust. Extreme temperatures can also affect the device’s performance, so keep it in a temperature-controlled area.
You can use protective cases when transporting the device to avoid accidental damage.
Routine Inspections
Technicians regularly check the tonometer’s parts, such as the probe, sensor, and screen, for signs of wear or damage. Early detection of issues can prevent more significant problems and ensure the device remains in optimal working condition.
Handheld Tonometers Are Transforming Eye Care
Portable tonometers revolutionize eye care by offering portable accuracy and ease of use. Modern eye exam tools are essential for reliable eye pressure testing and glaucoma screening in different healthcare environments.
The precision eye care tools available today reflect significant tonometry advancements and are a testament to ongoing ophthalmic innovation.
Invest in the future of eye care with a handheld tonometer from Nava Ophthalmic. Revolutionize your practice with portable eye care devices with unparalleled accuracy and ease of use.
Matthew Strachovsky, M.D.
Dr. Strachovsky's undergraduate training began in Boston, Massachusetts at Boston University and was completed at Stony Brook University in Long Island, NY. There he graduated Summa Cum Laude, obtaining a Bachelor of Science degree in Biology with special recognition for academic achievement.
He continued his education at Stony Brook School of Medicine and graduated with the additional designation of the "MD with Recognition" program. He worked as an intern in Internal Medicine at Winthrop University Hospital in NY and pursued a residency at Stony Brook University Hospital in Ophthalmology acting as Chief Resident in his final year. He completed his fellowship training in Vitreoretinal disease with a major emphasis on the diagnosis and management of retinal vascular diseases under the direction of Dr. Michael O'Brien at Koch Eye Associates in Rhode Island.
Dr. Strachovsky has presented research at the annual Association for Vision and Research in Ophthalmology meeting and published articles in journals including, Investigative Ophthalmology and Visual Science and The Journal of Neuro-ophthalmology.
Dr. Strachovsky's professional interests include the management of Age-Related Macular Degeneration and diabetic eye disease. He is Board Certified in Ophthalmology and a member of the American Academy of Ophthalmology, American Society of Retina Specialists, Young Ophthalmologist Network, and Leading Physicians of the World.
" I believe that the physician/patient relationship is more important than ever. Being an Ophthalmologist allows me to help patients and build a foundation of trust, knowledge, and professionalism when it comes to eye care".